Chronic Care Management (CCM)
The Centers for Medicare & Medicaid Services (CMS) recognizes care management as one of the critical components of primary care that contributes to better health and care for individuals, as well as reduced spending.
Beginning January 1, 2015, Medicare pays separately under the Medicare Physician Fee Schedule (PFS) under American Medical Association Current Procedural Terminology (CPT) code 99490, for non-face-to-face care coordination services furnished to Medicare beneficiaries with multiple chronic conditions.
Understanding CCM
Chronic Care Management (CCM) is defined as the non-face-to-face services provided to Medicare beneficiaries who have multiple (two or more), significant chronic conditions. In addition to office visits and other face-toface encounters (billed separately), these services include communication with the patient and other treating health professionals for care coordination (both electronically and by phone), medication management, and being accessible 24 hours a day to patients and any care providers (physicians or other clinical staff). The creation and revision of electronic care plans is also a key component of CCM.
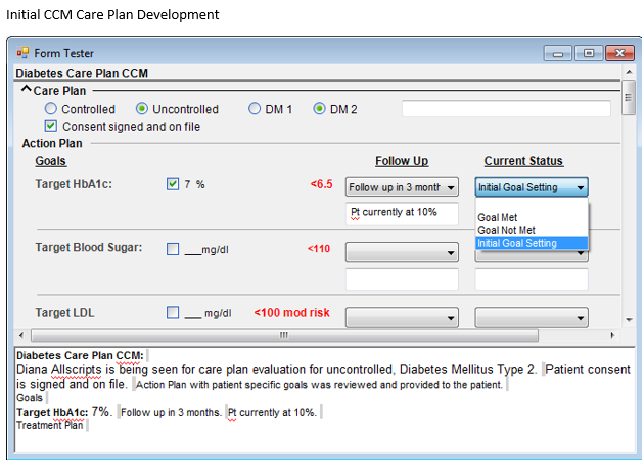
- The designated CCM clinician (MD, PA, NP) must establish, implement, revise, or monitor and manage an electronic care plan that addresses the physical, mental, cognitive, psychosocial, functional and environmental needs of the patient as well as maintain an inventory of resources and supports that the patient needs. Thus, the practice must use a certified EHR to bill CCM codes.
- Only one clinician can bill for any particular patient therefore it may be necessary to coordinate with the sub-specialists who may be providing a significant amount of care and treatment to one or more of the patient’s conditions. It will be important that the patients understand only one of their likely multiple physicians will be able to bill for CCM services.
Key Terms
- Eligible professional (EP) – The CCM codes can only be billed by a physician, advanced practice registered nurse, clinical nurse specialist, or physician assistant.
- Chronic condition – CPT states that patients must have “2 chronic continuous or episodic health conditions that are expected to last at least 12 months, or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline.” CMS did not provide guidance as to what diagnoses would meet this definition.
- Comprehensive Care Plan – This is an electronic summary of the physical, mental, cognitive, psychosocial, functional, and environmental assessments, a record of all recommended preventive care services, medication reconciliation with review of adherence and potential interactions and oversight of patient self-management of medications, an inventory of clinicians, resources, and supports specific to the patients, including how the services of agencies or specialists unconnected to the designated physician’s practice will be coordinated. Including assurance of care appropriate for patient’s choices and values.
- Clinical staff – Licensed clinical staff members (including APRN, PA, RN, LSCSW, LPN, clinical pharmacists, and “medical technical assistants” or CMAs) who are directly employed by the clinician (or the clinician’s practice) or a contracted third party and whose CCM services are generally supervised by the clinician, whether provided during or after hours. Thus the “incident to” rules do not necessarily require that the clinician be on the premises providing direct supervision.
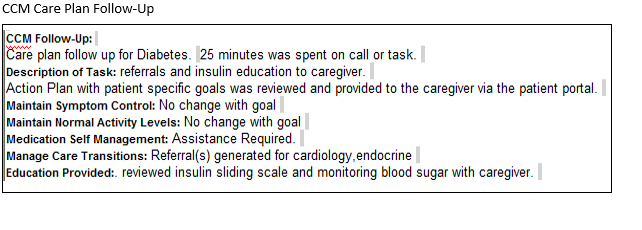
- Contact-based care – To count the time towards the 20-minutes of non-face-to-face time, the care must be “contact initiated.” This could be patient-doctor, patient-nurse, doctor-doctor, pharmacy-doctor, lab-doctor, or other contact regarding or by the patient via phone or electronic communication. General planning time or care coordination doesn’t count unless it is initiated based on a contact and/or results in a patient or patient-related contact. For example, if the pharmacist calls the office because the patient reported a rash, then the time counts. If the office spends time running a report of all participants due for a flu shot or an A1C check, that time doesn’t count. When they call and speak to the patient and then coordinate care, then that time would count. In-person visits, including group visits, do not count toward CCM codes.
- Certified CCM technology – For 2015, CCM codes must be provided by a certified EHR that satisfies either the 2011 or 2014 edition of the certification criteria for the EHR Incentive Programs with the following core technology capabilities:
- Structured recording of demographics, problems, medications, and medication allergies and
- Creation of a summary of care record that can be maintained and accessed at any time.
Billing
- CPT code 99490 – The 2015 average reimbursement is $42.60 adjusted based on geography.
- The practice must have the patient’s written consent in order to bill for CCM services (see Attachment 2).
- Only one clinician can furnish and be paid for CCM services during a calendar month. The clinician who is providing the primary care to the patient is the one who can bill. Usually this will be the primary care internist, but some specialists may be serving as the patient’s primary care physician.
- Copayments (coinsurance and deductibles) DO apply.
- The following codes cannot be billed during the same month as CCM (CPT 99490):
- Transition Care Management (TCM) – CPT 99495 and 99496
- Home Healthcare Supervision – HCPCS G0181
- Hospice Care Supervision – HCPCS G9182
- Certain ESRD services – CPT 90951-90970
- If other E&M or procedural services are provided, those services will be billed as appropriate. That time can NOT be counted toward the 20 minutes. If time, such as from a phone call, leads to an office visit resulting in an E&M charge, that time would be included in the billed office visit, NOT the CCM time.
Documentation
- Document patient consent, if they declined to participate, or indicated participation elsewhere (and if so, with whom).
- Document 20 minutes of non-face-to-face clinical staff time. Each practice will need to develop its own consistent system of documentation based on its unique physical, staffing, and EHR configuration. Consideration should include documentation of care provided by both internal and external (such as for call coverage) individuals, who and how care will be documented in the record, and how to document time spent doing different aspects of care and care coordination. It is quite possible that there will not be a CCM code billed for every patient every month, some months may not generate 20 minutes of care coordination.
- If after hours care is provided by a clinician who is not part of the practice, such as for call coverage, that individual must have access to the electronic care plan (other than by facsimile). The care plan may be accessed via a secure portal, a hospital platform, a web-based care management application, a health information exchange, or an EHR to EHR interface.
- Services can be provided “incident-to” the designated clinician if the CCM services are provided by licensed clinical staff employed by the clinician or practice who are under the general, not necessarily the direct, supervision of the designated clinician. The normal “incident-to” documentation requirements apply.
- Contracted clinicians, such as covering clinicians or locum tenens, count as long as they have access 24/7 to the patient’s electronic record and are under the general supervision of the CCM physician or “eligible practitioner.”